This is an operation normally performed for arthritis and occasionally ligament problems around the knee.

The knee acts as hinge joint and allows flexion (bending) and extension (straightening). The knee is formed by the tibiofemoral joints, where end of the femur (thigh bone) glides over the top of the tibia (shin bone) and the patellofemoral joint where the kneecap glides over the end part of the femur. The gliding surfaces of the knee are covered with articular cartilage which helps the joint to glide smoothly. Over time the articular cartilage can become damaged or ‘worn away’ and this is known as osteoarthritis.
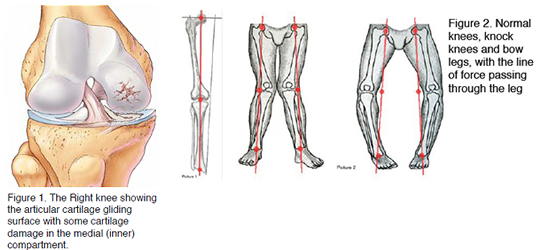
It is more common for the articular cartilage on the inside half of the knee to become damaged first and when this area alone is affected then it is known as medial compartment osteoarthritis. When the cartilage in all three compartments of the knee is damaged then this is known as tricompartmental osteoarthritis and this is not usually suitable for osteotomy surgery.
Most people with knee arthritis! Of all cases of knee arthritis presenting to surgeons, 75% predominantly involve the medial compartment. Patients who are born with varus knees (bow legs) are more likely to get medial compartment osteoarthritis. This is because the weight of their body mainly passes through the medial compartment of the knee rather than spreading the load evenly between the whole gliding surface of the knee.
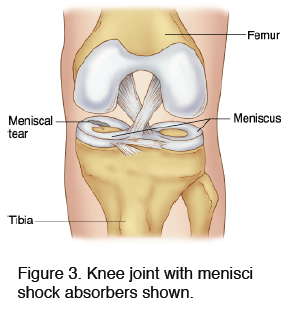
Other patients may have sustained an injury to the knee to initiate the damage to the cartilage in the medial compartment. This can happen after an injury to the crescent moon shaped shock absorbers in the knee known as menisci, particularly the medial meniscus. An injury to the ACL (Anterior Cruciate Ligament) can make the knee less stable and prone to cartilage damage over time. Osteoarthritis in association with cruciate ligament injury is frequently treated by osteotomy which can be used to help stabilize the knee by realignment.
Patients with medial compartment arthritis usually complain of pain and stiffness around the knee. They often point to the inside aspect of the knee as the main focus of their pain.
The knee can swell up particularly after strenuous activity and some patients will note grinding or locking of their knee.
Depending upon the degree of severity of the symptoms they may have difficulty doing their usual sporting activities such as running, or walking as far as normal.
Realigning the leg helps to take the pressure off the diseased medial compartment of the knee and relieve pain. Patients find walking and sporting activities easier. Realigning the limb at the stage when there is only osteoarthritis in one compartment is thought to dramatically slow and in some cases halt the spread of osteoarthritis throughout the rest of the knee joint. It is a useful alternative for patients who are still too young or active to consider a joint replacement. Occasionally a patient who has had osteotomy surgery will go on to develop osteoarthritis throughout the knee or simply suffers with severe pain. In such cases there is no barrier for the patient to have knee replacement surgery.
Osteotomy surgery is not widely performed in the UK, it has gone out of fashion as knee replacements became popular. However osteotomy surgery is still widely performed in Europe and there is a large body of evidence to support the practice. Mr Dawson has performed over 500 of these procedures with excellent results from longterm patient follow up.
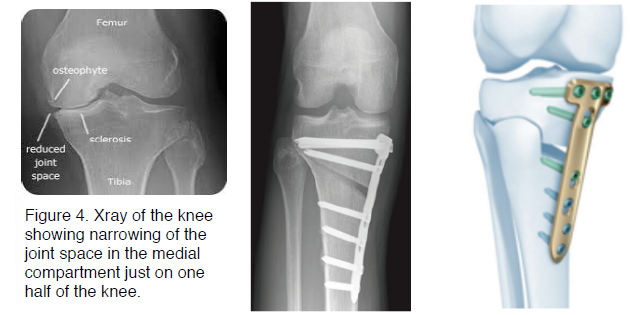
When you come to clinic we take a full patient history and examination along with standing X-rays of the knee joint and the patello-femoral joint. The X-ray will often show narrowing of the joint space in the medial compartment of the knee which suggest that a patient has medial compartment osteoarthritis.
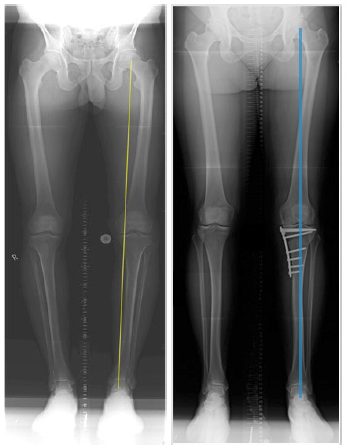
We will also perform an X-ray of the whole of both of your legs from the hip joints to the ankle joints, this allows us to carefully examine the overall alignment of your legs. We can calculate the weight bearing axis of your leg and find out where most of the force is passing through your knee joint.
Usually we will need to obtain an MRI scan which is done on a separate visit to the Radiology department. An MRI allows us to look at the menisci (the crescent moon shaped shock absorbers) to see if they are torn and will require attention at the time of surgery. It also allows us to check that the cartilage in the lateral compartment is in good condition and can withstand some extra force passing through it. After your MRI scan we will bring you back to clinic to discuss the results of the MRI and discuss treatment options.
We may offer certain patients a type of knee brace known as a medial offloading brace to trial. To a certain extent this mimics the result of osteotomy surgery by pushing the leg into a more normal alignment and taking the pressure of the damaged medial compartment. This is usually only a temporary solution whilst waiting for surgery. Patients who are overweight often find their knee pain is significantly improved when they lose weight. Simple analgesia such as paracetamol together with ibuprofen can help with pain and sleep disturbance form the pain.
An Osteotomy is a controlled surgical break or fracture of the bone to allow realignment of the limb. In the case of medical compartment osteoarthritis we perform an osteotomy in the tibia to realign the bow leg to being more straight or even slightly knock kneed (see figure 5). Usually we will start the procedure by performing an arthroscopy of the knee joint. This involves two tiny cuts at the front of the knee, one for the camera and one for the instruments. This allows us to identify and treat any meniscal tears or loose flaps of articular cartilage. After that we make two small incisions over the inside aspect of the leg just below the knee to allow us to perform a controlled osteotomy (fracture) of the top portion of the tibia and then gently wedge it open to realign the leg. The whole leg alignment X rays allow us to accurately calculate exactly how much to open up the wedge in order to realign the limb. Very occasionally it may be necessary to take bone graft usually from the wing of the pelvis to aid the healing of the osteotomy. We then use a strong titanium plate to hold the wedge open which is fixed onto the bone using screws. The skin is closed with clips and we apply dressings to cover the wounds.
Patients who smoke will be asked to quit as soon as possible. They must have stopped smoking at least 3 months before the procedure. Smoking has a profound effect on fracture healing and we must not risk the bone not healing back together. Patients will be seen in our pre-assessment clinic where an anaesthetic check up will be performed. They will also see one of the surgical team before the day of surgery to go through the consent form.
Patients arrive at 8am on the day of surgery. They should not eat from anything after midnight the night before, they can have water only up until 5am. The anaesthetist will come and discuss the plan with the patient. Most patients have their operation done under a spinal anaesthetic with some sedation. This involves an injection in the back to numb the legs which provides pain relief even after the operation has finished. The surgical team will answer any questions and mark the leg.
After theatre the patient will go to the recovery room and we will remove the bandages around the knee and apply a cryocuff to cool the knee and reduce swelling and pain. We use a special combination of medications before during and after the surgery to minimise the amount of bleeding, swelling and pain from the operation. Extra medications will be available on the chart to request if you feel pain or nausea. We call this enhanced recovery.
The physiotherapists will see you and help you to mobilise using crutches after the operation. For most patients they can put as much weight through the operated leg as the pain will allow, the plate will not break. The crutches are there as a support only.
In the first 2 weeks after the operation patients should aim to be at home not doing much and resting. You should employ a regular regime of ice application with elevation. You will be discharged from hospital with the cuff part of the Cryocuff device which when filled with water can be frozen and refrozen in the freezer. Please alternate this with other similar devices or even frozen peas but remember to place a tea towel or similar between the skin and the frozen device. There will be bruising and swelling around the knee and it will be sore.
On discharge from hospital you will have a 2 week course of clexane injections to thin the blood and reduce the risk of a DVT (deep vein thrombosis) whilst you are less mobile than usual. Please remember whilst you may be rightly informed that weight can be placed across your recovering limb it is not desirable nor a ‘badge of honour’ to walk any significant distances in this phase. Please concentrate on fully extending your knee and following the other physiotherapy exercises which have been prescribed.
The skin clips will be removed by your GP practice nurse at 12 days post op. The wound will usually look red around the margins due to the healing response. Any spreading redness up the leg combined with large swelling, fever or pus coming out of the wound is suggestive of infection and you should seek medical attention as a priority.
The physiotherapy team will continue to work with you as an outpatient and they provide us with a report at the 6 week mark post op. We will see you in clinic at the 3 month mark and perform repeat x rays of the limb to assess the correction. Routinely we then see patients at one year post op, to assess if they would benefit from having the plate removed. Patients will continue to see improvement in the knee symptoms over the year after their operation. Our patient database suggests that most patient’s symptoms continue to improve slowly long after that as well.
Download HTO (High Tibial Osteotomy) Physio Protocol
The usual port of call for minor problems should continue to be you GP.
Matt Dawson is a Specialist Knee Surgeon with over 16 years Consultant experience. Matt is internationally renowned as one of the leading authorities on knee realignment surgery
Specialist Knee Surgeon
Over 16 years Consultant experience
Internationally Recognised
Patient Centric Approach
Holistic Approach
Enhanced Recovery Programme (ERP)
Leading in Knee Realignment Surgery
Matt practices in the North of England and is available
to see patients from all over the UK
Circle Health group
Meadowside, Lancaster
Lancashire, LA1 3RH
Phone: 01524 62345
Fax: 01524 844725
Clayton Road,
Newcastle upon Tyne,
Tyne and Wear, NE2 1JP
Phone: 0191 281 6131
Cumbrian Knee Clinic @ Penrith
Community Hospital
Bridge Lane
Penrith, CA11 8HX
Phone: 01697 282119
Fax: 01697 282119








Copyright 2024 The Cumbrian Knee Clinic. All rights reserved.